Based on a talk by the same name given by Dr Gareth Parkes – Consultant Gastroenterologist @ the RCP Update, AMEX Stadium, 2019 – 20/03/2019
Our GI Microbiotic Makeup

Élie Metchnikoff won the nobel prize in 1908 for his discoveries about bacteria and immunology. After this he developed the theory that aging is caused by the build up of toxins in thegut. In an attempt to live forever he drank sour milk (Bulgarian Kaffir Yoghurt) every day. Unfortunately it didn’t work and he died at the age of 71 and was buried in Paris.
He however, is the great grandfather of this field and set about a chain reaction which leads up till today. In the 1990’s to early 2000’s we discovered that we are outnumbered 10 to 1 by our bacteria, but now what we have discovered & what a lot of people still don’t know is t
hat both our cells and the bacteria are probably outnumbered by the viruses harbored within the bacteria.
It is not yet clear what the role of these viruses are but the process of discovery so far has been much like zooming in on a google map of the Amazon. To continue the analogy we used to only be able to see the broad view of the microbiome & are only now zooming in on the roots:


![]()
Initially we could only culture the bacteria in a petri dish. Then we developed complex immunoflourescence assays. Now we have developed methods to look at the metabolome & transcriptome to assess the immune processes going on within the bacteria. It’s not just about the bacteria you produce, but also about what is going on inside them. We are only just starting to understand the impacts of this. The next stage will be looking at the virome and it’s implications.
The impacts of these processes are truly profound and affect your neurophysiology, neurohormonal functioning and cause some disease. Let’s take a look at how this has developed over time.
Your Microbiotia & Inflammatory Bowel Disease?
One of the earliest avenues for research exploration was ? E.Coli in macrophages – could this cause Crohn’s? After lots of research it was discovered that they didn’t.
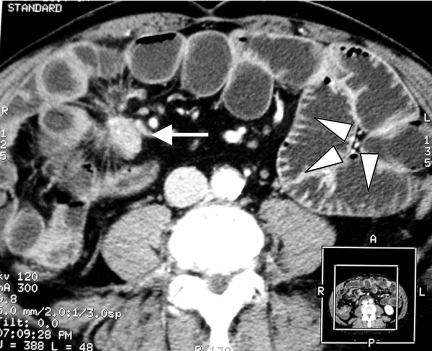
 Subsequent studies looking at bowel trauma and healing discovered that by re-biopsying previously biopsied colon it was possible to quantify the immunological response. In Crohn’s the healing response was subdued, unlike in UC patients or healthy controls. A similar response was found by injecting E.Coli into the arm. Healthy controls had a big peak in response, but in Crohn’s the response was subdued.
Subsequent studies looking at bowel trauma and healing discovered that by re-biopsying previously biopsied colon it was possible to quantify the immunological response. In Crohn’s the healing response was subdued, unlike in UC patients or healthy controls. A similar response was found by injecting E.Coli into the arm. Healthy controls had a big peak in response, but in Crohn’s the response was subdued.

Then several studies came out showing that the microbiota themselves become less diverse in UC/Crohn’s. This is pattern that continues throughout health – disease on a spectrum. You have low-risk individuals at one end with intact mucosal barriers, at-risk patients with perhaps a ‘leaky gut’ and other patients with Crohn’s/UC disease and complete mucosal failure asosciated with decrease in microbiomal diversity.
Other researchers have looked at whether fast food is causing the gut to become leaky? Transfats and inflammatory fats appear to disrupt this barrier and lead to dysbiosis. Dysbiosis subsequently predicts disease and biomarkers exist which can be used to map and anticipate this process to some degree.
 We have also found that in general a poor diet high in trans-fats can completely disrupt the baseline immunological state, leading to raised level of pro-inflammatory cytokines, increased baseline inflammatory response and higher risk for immune-mediated disease. This has particularly been demonstrated with high trans-fats in mice models.
We have also found that in general a poor diet high in trans-fats can completely disrupt the baseline immunological state, leading to raised level of pro-inflammatory cytokines, increased baseline inflammatory response and higher risk for immune-mediated disease. This has particularly been demonstrated with high trans-fats in mice models.
But how does this apply to humans and what can we do to treat these diseases?
Modulation – Probioitic
An analogy. Imagine a football stadium like this one this talk is being delivered in and the grass is your microbiome.

Pre-biotics are like fertilizer the grass while pro-biotics are like the new grass seeds.

Pre-biotics include dietary influences. There is good evidence that pre-biotics & dietary changes can be effective for IBS and possibly UC, but not so much in Crohn’s.
Regarding probiotics, their origin is steeped in history. In 1917 during the first world war one particular German trench crew got dysentery. All of them died except one individual. His microbiome was cultured and grew an organism – E.Coli Nissile which appears to confer some protection to E.Coli:

Following on from this over the years many new probiotics have been created, but only few have actually developed good evidence to support them. Recently the rules have changed and without this evidence they cannot be labelled as probiotics – sorry Yakult.
Several studies have more recently followed:
- Lactobacillus study – showed no improvement in the ability to metabolise alcohol.
- Bifidobacterial cultures in Japan – small reduction in visceral fat
- L.casei – Failed to improve immune responses to vaccination in healthy volunteers
- Nematodes have been made to live longer by probiotics
- Sad but not depressed people can possibly be helped by probiotics
- Rotavirus infections can definitely be shortened by the use of probiotics
- CD studies have shown no benefit for maintainence of remission
- In UC – VSL#3 trials showed some benefit. This definitely works in chronic pouchitis and was the first probiotic to be NICE approved.

Modulation – Faecal Microbiota Transplant (FMT)
If probiotics are the seeds, FMT is when you lay down entirely new turf!
Historical attempts have included the Japanese drinking ‘Yellow soup’ and the Berbers eating camel dung.
There are several successful studies, showing:
- FMT transplant in mice can make obese ones slim!
- In C-Difficile it categorically works. So much so, that the landmark study had to be stopped early at 43 out of 102 patients planned to be recruited. Diversity of the microbiome was also shown to improve.
- FMT doesn’t work in IBS – placebo is perhaps even better!
- Obesity – Vrieze et al 2012 demonstrated a 75% increase in insulin sensitivity using FMT, but further research is needed about the generalisability of this result.
- UC perhaps beneficial. Further trials are ongoing.




























You must be logged in to post a comment.