Disclaimer: This article is not intended as advice for patients but is intended as information for medical professionals only.
Firstly you have to establish the indication for transplant:

All the indications are listed here in this policy document but broadly they are broken down into:
- Chronic liver disease
- Hepatocellular Carcinoma
- Variant Syndrome
- National Appeals Panel

The UKELD score can be used to assess suitability for transplant. As the score reaches 49 this indicates a 9% one-year mortality rate and is the minimum criterion to be listed for transplantation. A score of 60 suggests 50% one-year mortality. Remember that these statistics were developed by looking at patients on the transplant list already so may not be applicable to new presentations.
HCC’s must be small
There are also a few pilot studies, including one for downstaging HCC’s which appeared to have a more indolent course. If patients are staged as ‘low risk’ for recurrence then they do benefit from transplantation but this is still in a pilot stage. There is also one for alcohol related liver disease but the criteria are so stringent that so far nobody has been transplanted on that pilot.
Assess the risk for that individual patient
In order to do this we need to look at survival. Every year in the UK about 2/3rds of patients are listed for transplant but around a third are deemed too unwell or needing other conservative treatment options first.
Biological factors are key and they will look at co-morbidities as well as several other factors. They will generally perform an echocardiogram, pulmonary function tests, blood gases, exercise capacity tests and some additional investigations for high risk patients. Nutrition will be assessed.
Outcomes are worse in those with BMI 40. Recent/current extrahepatic malignancy is an absolute contraindication. Tobacco smoking is a relative contraindication as it affects prognosis post-transplant.

In the UK, if people have gone back to drinking alcohol despite medical interventions within a medium-term time interval they are not transplantable. The point of stopping the alcohol is so that the liver can recover. The commonly held myth of the ‘6-month rule’ actually doesn’t exist in reality. Most of the guidelines instead talk about 2 years as an appropriate time interval, and the definition of absitinence is usually total. This advice needs to be clearly documented in the notes. Even a glass of wine at Christmas is not strictly allowed. Alcohol-free lager is also not allowed (as above)
This is because drinking even alcohol-free lager is a risk factor for relapse. Selective engagement in treatment is another risk factos for relapse; as is previous history, access to alcohol, underemployment, relationship factors, children, social support structures and personal motivation to engage in new habits.
There are also tests that can be used to detect whether or not people have been drinking alcohol. Increasingly cigarette smoking is being strongly discouraged as well because it is associated with poorer outcomes post-transplant.











 C
C
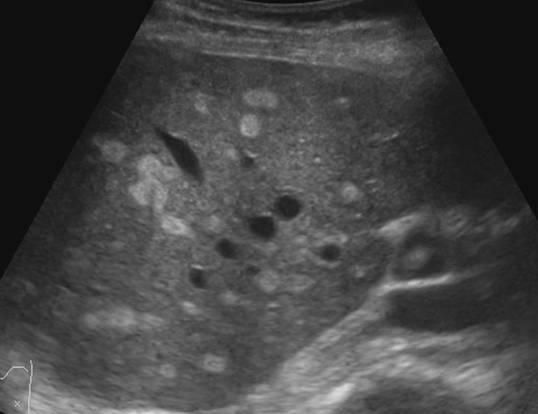
 This one above turned out to be a hyatid cyst (Echinococcosis).
This one above turned out to be a hyatid cyst (Echinococcosis).


You must be logged in to post a comment.