
Physiology – ‘A state of Loose tubes and high roids’
The foregut and small bowel speeds up transit of food contents. However, the large bowel slows down and this can lead to constipation, as can pressure of the baby on the rectosigmoid. They have very high levels of circulating steroid hormone.
Constipation
Increasing the fluid intake will often help. High fibre diet. Stop iron supplements and give reassurance.

Gastro Oesophageal Reflux Disease
Reflux becomes more common. Using salts, alginates, metoclopramide, sucralfate, H2 receptor antagonists and PPI’s can help.

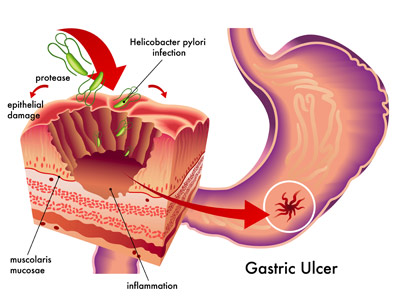
Peptic Ulcer Disease
This is relatively uncommon. Do not give misoprostol (Arthotec has misoprostol in it). Treatment is PPI / endoscopy in the context of bleeding
IBS
Do not investigate long-standing IBS, only proctoscopy if needed.

Try to minimise medication use unless absolutely necessary.

Abdominal Pain (unexplained – non-obstetric)
Can be appendicicits, pancreatitis, pyelonephritis, cholecystitis, pneumonia, renal colic, iliac vein thrombosis, Budd-Chiari and almost any cause. If you need to do a test then you should do it. However, at 8-15 weeks of gestation the risk of damaging a childs mental development with radiation is higher (>50mGy’s). This is about equivalent to two pelvic CT scans.
Liver Disease

Acute viral hepatitis and acute liver failure in pregnancy is still relatively uncommon in pregnant mothers. However, chronic hepatitis (normally hep B and C) need to be managed by specialists. Particularly as there is a risk of vertical transmission.
Acute hepatitis E however, is becoming a lot more common and comes with a 20% risk of acute fulminant liver failure in pregnancy.
Drugs
In general all pre-existing medication should be continued during pregnancy unless it is explicitly teratogenic as good chronic disease control is the most associated with good outcomes. Teratogenic medications should be changed to non-teratogenic ones in general. Beta-blockers can be used from the second trimester onwards in portal hypertension.
Inflammatory Bowel Disease
This has affects on fertility and pregnancy outcomes plus delivery options.

If you have UC – the disease is likely to reflect the pre-pregnant state (ie. if the UC was well controlled pre-pregnancy then it will tend to remain that way throughout).
Most exacerbations of inactive Crohn’s disease will occur during the first trimester. The vast majority of crohn’s patients will improve when pregnant. Fertility is more likely to be affected in crohn’s as it is strongly associated with prior surgery and the tubes may be involved.
Active disease at the time of conception is associated with an increased risk of miscarriage.

Acute flares should be treated aggressively and quickly. Medical treatment should be continued in general except for: Methotrexate, Thalidomide and 6-Thioguanine (no data) which are contraindicated [this is even the case for the partner]. Infliximab, Adalimumab, certolizumab, cyclosporin, tacrolimus, budesonide, metronidazole and ciprofloxacin are all probably safe in pregnancy. 5-ASA’s, sulfasalazine, azathioprine, corticosteroids and 6-mercaptopurine are all thought to be safe as long as folic acid supplementation is given.
When using biologic therapy there is some evidence that (infliximab/adalimumab) should be stopped after 30 weeks (third trimester) if possible. This is because of concerns Re: inducing immunosuppression in the infant.
Optimising maternal nutrition is also a major priority. Surgery should only be performed if absolutely necessary.
Previous ileostomy, colostomy is not a contraindication to normal full-term vaginal delivery.

However, c-section is indicated if the patient has severe peri-anal Crohn’s disease and some pouches (must be discussed with surgeons).