There is a fear that there is a lack of leadership within the NHS.
There is also a major difference between the current leading generation and those coming. The current generation is very traditional. In general the current leading generation will stick to what worked before and just keep going. The coming generation want instant feedback, (my generation stands in the gap but I lean toward the millenial side).
This new generation poses a significant threat to the new generation and can make it difficult to relate. If the design of the workforce has been performed by the older generation it will be the younger generation which will have to live with it.
You can either be an ostrich, king Cnut or a surfer. Click the pictures to see what they each do?

Ostriches hide from the sea

King Cnut tried to stop it

Surfers observe it and try to catch the wave
There are all sorts of regulatory bodies including NHS England, CQC, CCG’s, Dept for Health, HEE, NHSi and all sorts of other groups within the NHS. They each have different focuses and each try to get things ready for the future.
They are all working to this 5 year forward view plan. This involves commissioning of services (a mechanism involving competing for contracts and payment for services ‘commissioned’, networks are being built to try and connect different services (ie. Diabetes) to try and save money. Often the money is given in ‘packets’ which have to be spent quickly. You can build business cases which are ready to go at the drop of a hat to try and access this money.
Then there are clinical senates. These are groups led by clinicians to provide multidisciplinary input to strategic clinical decision-making. The groups, 12 of which are due to be established, should help to provide clinical input to the other decision making bodies.
The five year forward view contains the following chapters:
- Chapter One – Why will the NHS need to change?
- Chapter Two – What will the future look like?
A new relationship with patients and communities, Getting serious about prevention, Empowering patients, Engaging communities, The NHS as a social movement
- Chapter Three – What will the future look like?
New models of care – Emerging models, One size fits all? New care models, How we will support local co-design and implementation
- Chapter Four – How can we get there?
We will back diverse solutions and local leadership, We will create aligned national NHS leadership, We will support a modern workforce, We will exploit the information revolution, We will accelerate useful health innovation, We will drive efficiency and productive investment.

Prevention is much more important than cure. This has to become top priority if we are to change the NHS structure and culture and ultimately reduce costs.
Motivational interviewing, telehealth (Airedale model worked), urgent and emergency care networks, enhanced care in care homes. Multispecialty community providers, primary and acute care systems.
Heavy investment in general practice. 5,000 extra GP’s and 3,000 extra mental health practitioners.
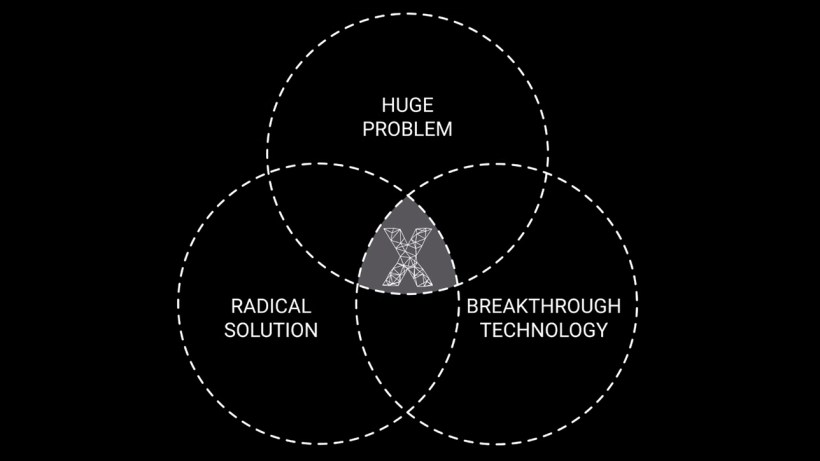
Then we discussed trappist monks (as below). August Turak’s book shows that the key factors needed for success are: clarity of mission, faith in the mission, service and selflessness, commitment to excellence and trust. Does your organisation have these factors?
Will the NHS have this clear why? This is what the FTP’s are about. Joining up care and having a common vision.
Speakers ending comment: Think creatively, learn to play the game and you can surf the waves and succeed to make healthcare better for patients.

































You must be logged in to post a comment.